![]()
The Liver-Brain Axis
Dr Anna Hadjihambi
Dr Anna Hadjihambi has been awarded a UKRI Future Leaders Fellowship to establish her independent multidisciplinary research programme at the Roger Williams Institute of Liver Studies, in collaboration with KCL (Adjunct Honorary Lecturer) and UCL (Honorary Lecturer).
Anna is group leader of the Liver-Brain Axis group and the aim of their research is to investigate the pathological mechanisms underlying the detrimental effects of metabolic dysfunction associated steatotic liver disease (MASLD) on the brain. Using analysis of human biomedical data and experimental models, the Hadjihambi group focuses on understanding whether cerebrovascular alterations are responsible for the impaired brain function associated with MASLD and whether they develop as a result of disease-induced autonomic dysfunction. Understanding the underlying mechanisms has an added value as it is currently unclear whether cerebrovascular alterations are reversible following weight loss and MASLD resolution.
With the mean age of global MASLD prevalence being ~50 years old, this is especially relevant as autonomic and vascular dysfunction develops spontaneously with age and progresses to severely impact quality of life, adding to the burden of care, as well as increasing the risk of neurodegenerative diseases. This research programme further investigates whether the impact of MASLD-induced cerebrovascular remodelling on brain function is most prominent during ageing. Anna is also co-supervising a PhD project funded by the Neuro-Immune Interactions in Health & Disease Wellcome Trust PhD Programme, investigating the potential impact of gut-derived systemic inflammation as a driver of cerebral dysfunction in MASLD.
Being a strong supporter of collaborative research, Anna has several national and international collaborators, and her group contributes to various studies from different disciplines (cardiovascular, pharmacology, neuroscience and physiology). Additionally, Anna is a STEM ambassador, Greek Women in STEM Mentor, the secretary of the International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN), co-chair of the ISHEN Translational committee and Associate Editor of the npj Gut and Liver journal.
X (Twitter)
LinkedIn
ORCID
Research:
Dr Hadjihambi’s translational research focuses on dissecting the molecular mechanisms linking chronic liver disease to brain dysfunction, accelerated brain ageing and neurodegenerative conditions. The main project of the group uses state-of-the-art in vivo, molecular and imaging techniques, combined with human data analysis in order to investigate the pathological mechanisms underlying the effects of NAFLD on the cerebrovascular and brain function. The aim is to obtain knowledge that will lead to the development of novel and effective neuroprotective therapies.
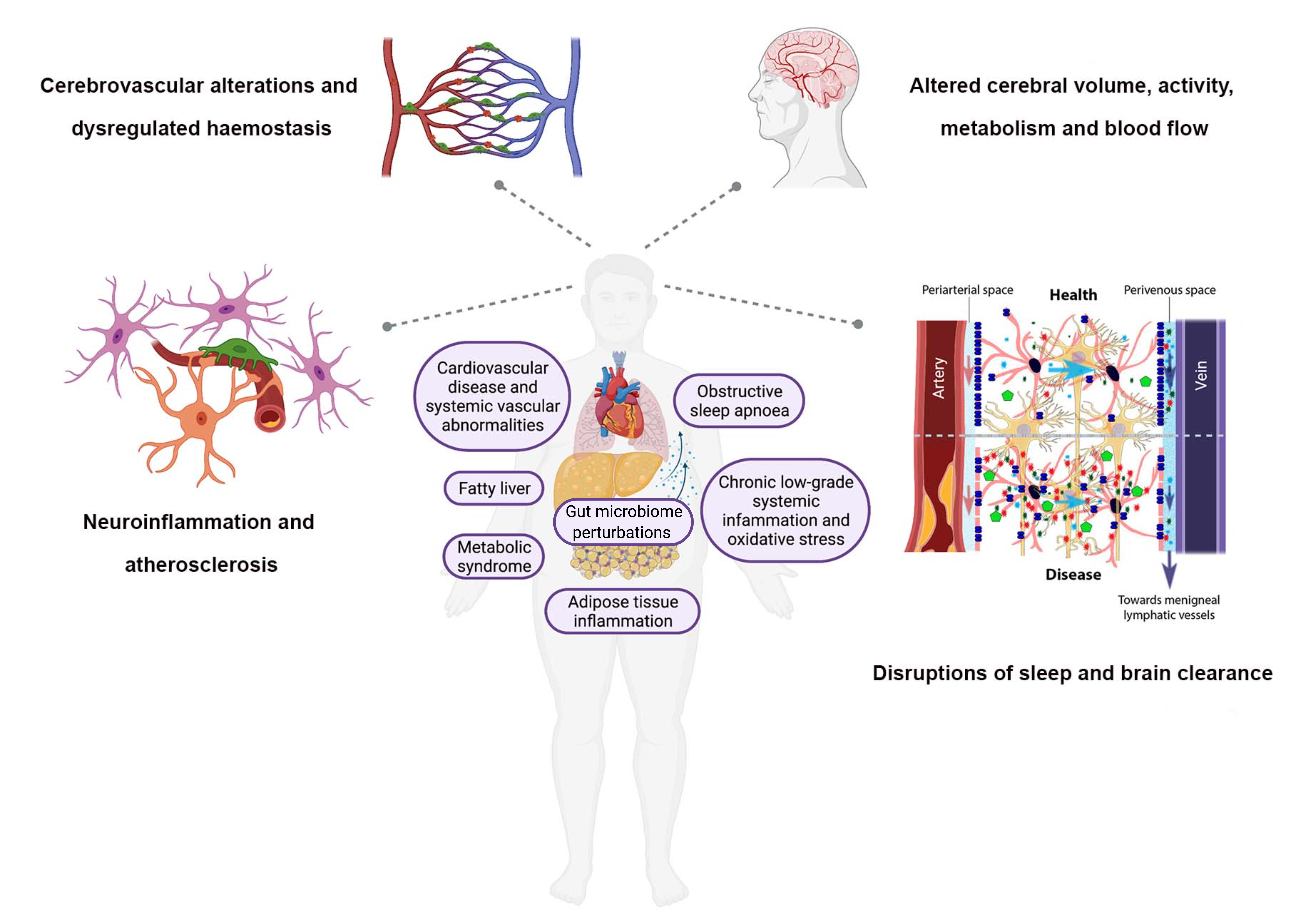
Schematic diagram summarising factors, contributing to the pathogenesis of NAFLD and possibly increasing the risk of development and progression of neurodegenerative diseases.
Projects:
- “Is fatty liver disease increasing our risk of developing neurodegenerative conditions?” This project addresses the hypothesis that gut microbiome perturbations in NAFLD/NASH will induce systemic and brain inflammation lowering the threshold for developing diseases like Parkinson’s and Alzheimer’s disease.
- Understanding the mechanisms underlying NAFLD-associated brain dysfunction and the potential of its reversibility following liver disease resolution during ageing.
Key collaborations:
- Dr Vishal Patel: Development of novel non-invasive methods for the diagnosis of hepatic encephalopathy
- Dr Antonio Riva: Bacterial translocation and brain dysfunctions in liver disease
Team:
- Christos Konstantinou | Laboratory Technician
- Matthew Siddle | Neuro-Immune Wellcome Trust PhD Programme
Key publications:
- Hadjihambi A., Konstantinou C., Klohs J., Monsorno K., Guennec L. A., Donnelly C., et. al. 2022. Partial MCT1 invalidation protects against diet-induced non-alcoholic fatty liver disease and the associated brain dysfunction. J Hepatol; 78 (1): 180-190. https://doi.org/10.1016/j.jhep.2022.08.008.
- Hadjihambi A. 2021. Cerebrovascular alterations in NAFLD: Is it increasing our risk of Alzheimer’s disease?. Anal Biochem, 636: 114387. https://doi.org/10.1016/j.ab.2021.114387
- Hadjihambi A., Pierzchala K., Cudalbu C., Simicic D., Donnelly C., Konstantinou C., et. al. 2022. Ammonia impairs brain oxygenation in an animal model of minimal hepatic encephalopathy. J Hepatol Reports; 4 (8): 100509. https://doi.org/10.1016/j.jhepr.2022.100509
- Hadjihambi, A., Karagiannis, A., Theparambil, S. M., Ackland, G. L. & Gourine, A. V. 2020. The effect of general anaesthetics on brain lactate release. Eur J Pharmacol; 881:173188. https://doi.org/10.1016/j.ejphar.2020.173188
- Hadjihambi A., Harrison I. F., Costas-Rodriguez M., Vanhaecke F., Arias N., Gallego-Duran R., et al. 2018. Impaired brain glymphatic flow in experimental hepatic encephalopathy. J Hepatol;70(1):40-49. https://doi.org/10.1016/j.jhep.2018.08.021
- Hadjihambi, A., De Chiara, F., Hosford, P. S., Habtetion, A., Karagianis, A., Davies, H., et al. 2017. Ammonia mediates cortical hemichannel dysfunction in rodent models of chronic liver disease. Hepatology, 65, 1306-1318. https://doi.org/10.1002/hep.29031
- Gallego-Durán R.*, Hadjihambi A.* Ampuero J., Rose F. C., Jalan R.** & Romero-Gómez M.** 2024. Ammonia-induced stress response in liver disease progression and hepatic encephalopathy, Nat. Rev. Gastroenterol. Hepatol; 21, 774–791
- Hadjihambi A.,* Velliou R.,* et al.. 2023. Novel In Vivo Micro-Computed Tomography Imaging Techniques for Assessing the Progression of Non-Alcoholic Fatty Liver Disease. J. Vis. Exp. (193), e64838, DOI: 10.3791/64838